Using Waiver Supports and Services
Eligibility for Waiver Services
In order to be eligible for services funded through Waivers, a person must meet the following criteria:
- Have a diagnosis of developmental disability,
- Meet Medicaid financial eligibility,
- Meet the Level of Care Criteria as determined by the Virginia Individual DD Eligibility Survey (VIDES), and
- Accept services within 30 days.
The criteria for Waiver eligibility include: diagnostic, financial, and functional.
Eligibility Determination and Slot Assignment
In order to use services through the Waivers, a person needs to be determined eligible for services and assigned a slot. There are a limited number of slots and everyone who is eligible does not get to receive services right away. If a slot is not available, the SC determines the individual’s priority needs level and places the person’s name on the waiting list via Virginia Waiver Management System (WaMS). A Critical Needs Summary documenting the person’s level of urgency is also completed by the SC.
When a slot becomes available, the DBHDS-supported regional committee will assign the slot to the person on the waiting list who is found to have the greatest need for services.
Determination of Support
When someone is determined eligible and a slot is available, the level of support needed is assessed. A tool that is used to determine individual support levels is the Supports Intensity Scale® (SIS) The SIS® measures support needs in the areas of home living, community living, lifelong learning, employment, health and safety, social activities, and protection and advocacy. It is administered by qualified, trained interviewers.
The DDS electronic service authorization system is called WaMS (Waiver Management System).
Support Coordination
Each person who is enrolled in a Waiver is assigned a support coordinator (SC). SCs work for or contract with the CSB that serves the area in which the person lives. The SC is responsible for linking the person with service providers, as well as coordinating and monitoring the services. The SC, Waiver service providers, the person’s family members and others he/she chooses, meet together to help him/her develop an Individual Support Plan (ISP).
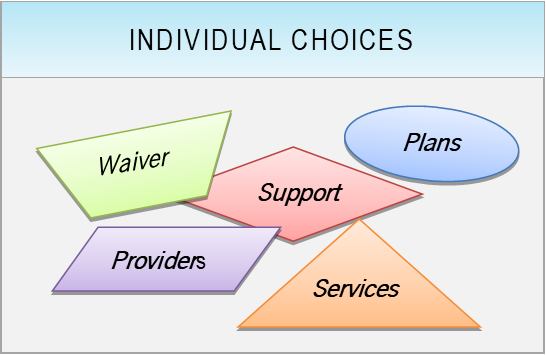
Choice
Eligible individuals for whom a slot is available must be allowed to choose:
- Whether they want to participate in the Waiver program,
- What services they will receive,
- Who the service provider(s) will be,
- What’s in their plan, and
- The supports to be provided.
Considerations in Community Settings
The Home and Community-Based Services (HCBS) settings regulations became effective in March 2014. The regulations are designed to enhance the quality of HCBS, provide additional protections, and ensure full access to the benefits of community living. They establish requirements for the qualities of settings where individuals live and/or receive Medicaid-reimbursable HCBS services. The rules focus on the quality of individuals’ experiences so that people receiving Medicaid-funded HCBS have services that protect individual choice and promote community integration.
Service Authorization
All Waiver services must be authorized by the Division of Developmental Services (DDS) prior to the start of services. The SC must review service providers’ service plans (called Plans for Supports) to ensure that the plans match what was decided at the planning meeting. The SC also ensures that the individual’s choices are the focus and driving force of the plan prior to requesting authorization. Changes in type and amount of services can be made only with prior authorization from DDS.